Major risks associated with adolescent cannabis use.
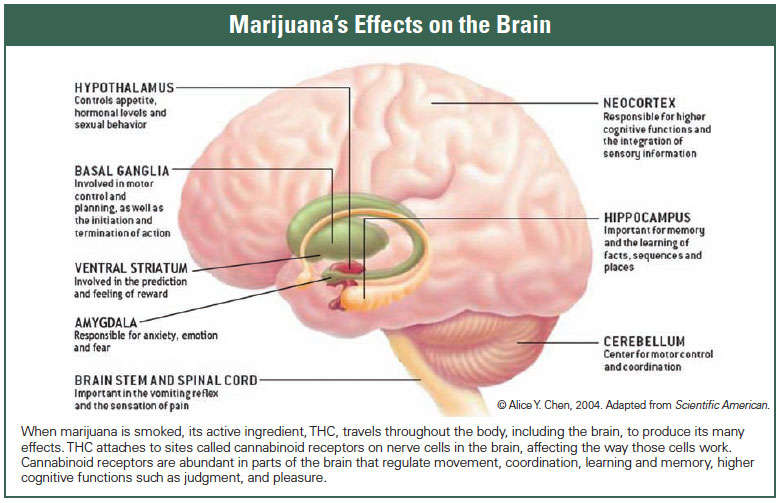
There are several unique risks that have emerged over the past few years associated with cannabis use among adolescents. As our understanding of the development of the human brain has increased, so too has the potency of THC – the main psychoactive component in cannabis – which has increased by up to 400% over the past fifty years. Science has explored how this increase in potency could potentially impact brain development among our student-aged population, which continues until their mid-twenties. Although rates of cannabis use among youth ages 15-24 in Canada continue to decrease, approximately 25% reported having used cannabis with the average age of initiation being 14 years-old. We cannot yet conclude how cannabis legalization for adults in Canada will impact youth consumption, but data from Washington and Colorado have not shown a significant increase in cannabis use among those under the U.S. legal age of 21.
Here are three major risks associated with adolescent cannabis use:
1. LOWER SCHOOL PERFORMANCE
Studies have shown that an individual’s working memory is impacted by cannabis use, with the effects potentially lasting for several days. This could impact a student’s academic performance and cause them to fall behind. As well, unlike alcohol, there is evidence that the effects of cannabis can persist over years of regular and continued use. These include the potential for a lowering of inhibition and reasoning skills, and a reduction in memory performance. Research has also shown that regular cannabis use could result in lower levels of educational attainment, including lowering high school graduation rates.
2. PSYCHOSIS
Cannabis use can result in psychotic episodes, where some youth lose touch with reality. These effects can last anywhere from a few hours to a few days, but do eventually resolve. However, in instances where heavy or frequent use is combined with beginning cannabis use at a younger age, there can be as much as a twofold increased risk of developing a chronic psychotic disorder, especially where there is a family history of schizophrenia.
3. CANNABIS USE DISORDER (CUD)
One-in-six youth who experiment with cannabis will go on to develop Cannabis Use Disorder (CUD). This can result in a reduction in grades, increased conflict at home, and changes within the student’s social circle of friends – with these changes often occurring over the course of a single year’s time. According to research, approximately 3% of older male high school students have CUD.
While cannabis has a long history of human use, recent scientific findings have discovered more about the developing adolescent brain and specific areas that are vulnerable to cannabis. For adolescents who use cannabis daily or weekly, studies have pinpointed functional brain deficits that require them to compensate by working harder than those who are not regular users. Fostering an open-door policy and being non-judgemental can help begin important conversations with students on these serious risks.
REFERENCES
Morin JF, Afzali MH, Bourque J, Stewart SH, Sequin JR, O’Leary-Barrett MA, Conrod PJ. Population-Based Analysis of the Relationship Between Substance Use and Adolescent Cognitive Development. Am J of Psych 2018, e-published.
Morean ME, Kong G, Camenga DR, Cavallo DA, Krishnan-Sarin S. High school students’ use of electronic cigarettes to vaporize cannabis. Pediatrics 2015;136(4):611–6.
Friese B, Slater MD, Annechino R, Battle RS. Teen use of marijuana edibles: A focus group study of an emerging issue. J Prim Prev 2016;37(3):303–9.
Morgan CJ, Noronha LA, Muetzelfeldt M, Feilding A, Fielding A, Curran HV. Harms and benefits associated with psychoactive drugs: Findings of an international survey of active drug users. J Psychopharmacol 2013;27(6):497–506.
Rieder MJ; Canadian Paediatric Society, Drug Therapy and Hazardous Substances Committee. Is the medical use of cannabis a therapeutic option for children? Paediatr Child Health 2016;21(1):31–4.
WHO. Social Determinants of Health and Well-being Among Young People. Health Behaviour in School-Aged Children (HBSC) Study: International Report From the 2009/2010 Survey. Copenhagen: WHO Regional Office for Europe, 2012.
Health Canada. Canadian Alcohol and Drug Use Monitoring Survey (CADUMS): Canadians Aged 15 Years and Older. 2012. http://www.hc-sc.gc.ca/hc-ps/drugsdrogues/stat/_2012/summary-sommaire-eng.php (Accessed September 19, 2016).
Brunelle N, Plourde C, Landry M, et al. Patterns of psychoactive substance use among youths in Nunavik. Indittera 2010;2:1–12.
Colorado Department of Public Safety. Marijuana Legalization in Colorado: Early Findings; A Report Pursuant to Senate Bill 13–283. March 2016. http://cdpsdocs.state.co.us/ors/docs/reports/2016-SB13-283-Rpt.pdf (Accessed September 19, 2016).
Roffman R . Legalization of cannabis in Washington state: How is it going? Addiction 2016;111(7):1139–40.
Giedd JN, Blumenthal J, Jeffries NO, et al. Brain development during childhood and adolescence: A longitudinal MRI study. Nat Neurosci 1999;2(10):861–3.
Lenroot RK, Giedd JN. Brain development in children and adolescents: Insights from anatomical magnetic resonance imaging. Neurosci Biobehav Rev 2006;30(6):718–29.
Hurd YL, Michaelides M, Miller ML, Jutras-Aswad D. Trajectory of adolescent cannabis use on addiction vulnerability. Neuropharmacology 2014;76(Pt B):416–24.
George T, Vaccarino F, eds. Substance Abuse in Canada: The Effects of Cannabis Use During Adolescence. Ottawa: Canadian Centre on Substance Abuse, 2015.
Blakemore SJ. Teenage kicks: Cannabis and the adolescent brain. Lancet 2013;381(9870):888–9.
Anderson VA, Anderson P, Northam E, Jacobs R, Catroppa C. Development of executive functions through late childhood and adolescence in an Australian sample. Dev Neuropsychol 2001;20(1):385–406.
Bossong MG, Niesink RJ. Adolescent brain maturation, the endogenous cannabinoid system and the neurobiology of cannabis-induced schizophrenia. Prog Neurobiol 2010;92(3):370–85.
Lisdahl KM, Wright NE, Kirchner-Medina C, Maple KE, Shollenbarger S. Considering cannabis: The effects of regular cannabis use on neurocognition in adolescents and young adults. Curr Addict Rep 2014;1(2):144–56.
Jager G, Block RI, Luijten M, Ramsey NF. Cannabis use and memory brain function in adolescent boys: A cross-sectional multicenter functional magnetic resonance imaging study. J Am Acad Child Adolesc Psychiatry 2010;49(6):561–72.e3.
Cascini F, Aiello C, Di Tanna G. Increasing delta-9-tetrahydrocannabinol (?-9-THC) content in herbal cannabis over time: Systematic review and meta-analysis. Curr Drug Abuse Rev 2012;5(1):32–40.
Karila L, Roux P, Rolland B, et al. Acute and long-term effects of cannabis use: A review. Curr Pharm Des 2014;20(25):4112–8.
Li MC, Brady JE, DiMaggio CJ, Lusardi AR, Tzong KY, Li G. Marijuana use and motor vehicle crashes. Epidemiol Rev 2012;34:65–72.
Papafotiou K, Carter JD, Stough C. The relationship between performance on the standardised field sobriety tests, driving performance and the level of delta9tetrahydrocannabinol (THC) in blood. Forensic Sci Int 2005;155(2–3):172–8.
Ramaekers JG, Robbe HW, O’Hanlon JF. Marijuana, alcohol and actual driving performance. Hum Psychopharmacol 2000;15(7):551–8.
Hartman RL, Brown TL, Milavetz G, et al. Cannabis effects on driving lateral control with and without alcohol. Drug Alcohol Depend 2015;154:25–37.
Canadian Council of Motor Transport Administrators. Public Opinion Survey on Drugs and Driving – Summary Report. http://ccmta.ca/images/publications/pdf//CCMTA_Public_Opinion_Survey_of_Drugs_and _Driving_in_Canada_revised_2014_04_14_FINAL_ENGLISH.pdf (Accessed September 26, 2016).
Smith-Kielland A, Skuterud B, Mørland J. Urinary excretion of 11-nor-9-carboxy-delta9tetrahydrocannabinol and cannabinoids in frequent and infrequent drug users. J Anal Toxicol 1999;23(9):323–32.
Wang GS, Le Lait MC, Deakyne SJ, Bronstein AC, Bajaj L, Roosevelt G. Unintentional pediatric exposures to marijuana in Colorado, 2009–2015. JAMA Pediatr 2016;170(9):e160971.
Turner SD, Spithoff S, Kahan M. Approach to cannabis use disorder in primary care: Focus on youth and other high-risk users. Can Fam Physician 2014;60(9):801–8, e423–32.
Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med 2014;370(23):2219–27.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th edn. Arlington: APA, 2013.
Budney AJ, Hughes JR. The cannabis withdrawal syndrome. Curr Opin Psychiatry 2006;19(3):233–8.
Georgiades K, Boyle MH. Adolescent tobacco and cannabis use: Young adult outcomes from the Ontario child health study. J Child Psychol Psychiatry 2007;48(7):724–31.
Merline A, Jager J, Schulenberg JE. Adolescent risk factors for adult alcohol use and abuse: Stability and change of predictive value across early and middle adulthood. Addiction 2008;103(Suppl 1):84–99.
Suris JC, Akre C, Berchtold A, Jeannin A, Michaud PA. Some go without a cigarette: Characteristics of cannabis users who have never smoked tobacco. Arch Pediatr Adolesc Med 2007;161(11):1042–7.
Degenhardt L, Coffey C, Carlin JB, Swift W, Moore E, Patton GC. Outcomes of occasional cannabis use in adolescence: 10-year follow-up study in Victoria, Australia. Br J Psychiatry 2010;196(4):290–5.
Bélanger RE, Akre C, Kuntsche E, Gmel G, Suris JC. Adding tobacco to cannabis–its frequency and likely implications. Nicotine Tob Res 2011;13(8):746–50.
Bélanger RE, Marclay F, Berchtold A, Saugy M, Cornuz J, Suris JC. To what extent does adding tobacco to cannabis expose young users to nicotine? Nicotine Tob Res 2013;15(11):1832–8.
Vandrey RG, Budney AJ, Hughes JR, Liguori A. A within-subject comparison of withdrawal symptoms during abstinence from cannabis, tobacco, and both substances. Drug Alcohol Depend 2008;92(1–3):48–54.
Zimmermann P, Wittchen HU, Waszak F, Nocon A, Höfler M, Lieb R . Pathways into ecstasy use: The role of prior cannabis use and ecstasy availability. Drug Alcohol Depend 2005;79(3):331–41.
Beck F, Legleye S, Spilka S. Multiple psychoactive substance use (alcohol, tobacco and cannabis) in the French general population in 2005. Presse Med 2008;37(2 Pt 1):207–15.
Bebarta VS, Ramirez S, Varney SM. Spice: a new “legal” herbal mixture abused by young active duty military personnel. Subst Abus 2012;33(2):191–4.
National Conference of State Legislatures. Synthetic Cannabinoids (Aka “K2”/“Spice”) Enactments. Washington, 2012.
Patton GC, Coffey C, Carlin JB, Degenhardt L, Lynskey M, Hall W. Cannabis use and mental health in young people: Cohort study. BMJ 2002;325(7374):1195–8.
Rubino T, Zamberletti E, Parolaro D. Adolescent exposure to cannabis as a risk factor for psychiatric disorders. J Psychopharmacol 2012;26(1):177–88.
Rey JM, Sawyer MG, Raphael B, Patton GC, Lynskey M. Mental health of teenagers who use cannabis. Results of an Australian survey. Br J Psychiatry 2002;180:216–21.
Meier MH, Hall W, Caspi A, et al. Which adolescents develop persistent substance dependence in adulthood? Using population-representative longitudinal data to inform universal risk assessment. Psychol Med 2016;46(4):877–89.
Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, Lewinsohn PM. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. J Psychiatr Res 2008;42(3):230–9.
Cornelius JR, Kirisci L, Reynolds M, Clark DB, Hayes J, Tarter R . PTSD contributes to teen and young adult cannabis use disorders. Addict Behav 2010;35(2):91–4.
Johns A. Psychiatric effects of cannabis. Br J Psychiatry 2001;178:116–22.
D’Souza DC, Perry E, MacDougall L, et al. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: Implications for psychosis. Neuropsychopharmacology 2004;29(8):1558–72.
Arendt M, Rosenberg R, Foldager L, Perto G, Munk-Jørgensen P. Cannabis-induced psychosis and subsequent schizophrenia-spectrum disorders: Follow-up study of 535 incident cases. Br J Psychiatry 2005;187(6):510–5.
Moore TH, Zammit S, Lingford-Hughes A et al. Cannabis use and risk of psychotic or affective mental health outcomes: A systematic review. Lancet 2007;370(9584):319–28.
Radhakrishnan R, Wilkinson ST, D’Souza DC. Gone to pot—a review of the association between cannabis and psychosis. Front Psychiatry 2014;5:54.
Large M, Sharma S, Compton MT, Slade T, Nielssen O. Cannabis use and earlier onset of psychosis: A systematic meta-analysis. Arch Gen Psychiatry 2011;68(6):555–61.
Di Forti M, Sallis H, Allegri F, et al. Daily use, especially of high-potency cannabis, drives the earlier onset of psychosis in cannabis users. Schizophr Bull 2014;40(6):1509–17.
Lynskey MT, Coffey C, Degenhardt L, Carlin JB, Patton G. A longitudinal study of the effects of adolescent cannabis use on high school completion. Addiction 2003;98(5):685–92.
Brook JS, Stimmel MA, Zhang C, Brook DW. The association between earlier marijuana use and subsequent academic achievement and health problems: A longitudinal study. Am J Addict 2008;17(2):155–60.
Fergusson DM, Horwood LJ, Beautrais AL. Cannabis and educational achievement. Addiction 2003;98(12):1681–92.
Jackson NJ, Isen JD, Khoddam R, et al. Impact of adolescent marijuana use on intelligence: Results from two longitudinal twin studies. Proc Natl Acad Sci USA 2016;113(5):E500–8.
Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci USA 2012;109(40):E2657–64.
Fergusson DM, Boden JM. Cannabis use and later life outcomes. Addiction 2008;103(6):969–76; discussion 977–8.
Schweinsburg AD, Brown SA, Tapert SF. The influence of marijuana use on neurocognitive functioning in adolescents. Curr Drug Abuse Rev 2008;1(1):99–111.



One thought on “Cannabis: What are the risks for youth?”